Diabetic nerve pain, or diabetic neuropathy, is a serious complication of diabetes. High glucose levels can damage nerve fibers throughout our entire body, especially in our feet and legs. Also, it can cause pain and numbness.
But, this nerve damage can lead to problems with our urinary tract, digestive system, heart, and blood vessels. Symptoms can range from mild to severe.
Even though it’s difficult to treat, we can reduce the symptoms and slow down its progression. We can do that with a healthy lifestyle and control over our blood sugar levels.
The Groundbreaking Study
Recently, NCBI conducted by researchers from King’s College London discovered the molecular basis of diabetic nerve pain. Although it involved only mice, the findings can lead to possible treatment that targets the source of diabetic nerve pain.
High blood sugar causes painful diabetic neuropathy to one in four individuals with diabetes. Symptoms include shooting pain, prickling and tingling sensations, and extreme sensitivity to touch in the hands and feet which can progress into arms and legs.
All this can lead to impaired mobility, obesity, and other diabetes complications.
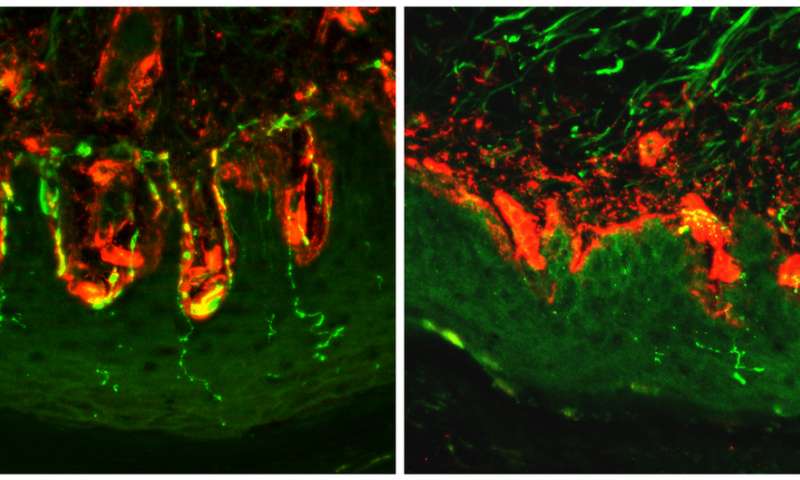
The molecular causes of diabetic neuropathy are not well understood which is why this condition is hard to treat. But, the new study gives the first proof that HCN2 – a protein molecule – could be the cause of diabetic nerve pain.
Over-activity of this protein molecule resulted in a pain sensation in mice with diabetes. What’s more, researchers discovered that removing the HCN2 from pain-sensitive nerve fibers or blocking its activity can stop the pain sensation completely.
The senior author, Peter McNaughton, says the rise of obesity has led to a rise in type 2 diabetes.
Since one in four of those with diabetes develops diabetic neuropathy, the lack of effective treatment makes all of them resign to a life of continuous suffering.
But, the study discovers the molecular mechanism that causes pain in animals. This increases the chances of discovering new treatments for diabetic neuropathy in those with diabetes.
Conclusion
The first author of the study, Dr. Christoforos Tsantoulas, explains that for now, they don’t have selective medications that can suppress the activity of this protein molecule without interfering with other functions in the body, like regulation of the heart rate.
However, the study encourages the creation of targeted pain medication that can block this protein molecule without affecting other molecules’ activity.
Source Medical Express | Mayo Clinic

